High Value Practice Alliance
As the cost of health care in the United States continues to rise, of utmost concern are reports that medical bills are creating substantial hardships for patients and that the cost of health care is now the biggest financial concern facing American families. Health care debt is a leading driver of personal bankruptcy and home foreclosure. Both insured and uninsured patients are burdened by medical bills. Confounding these issues is evidence that patients avoid necessary care (prescription refills, doctors appointments) because of cost. In response to these challenges, providers across the country are reflecting on their practice to identify opportunities and implement initiatives that improve patient care quality and safety while reducing costs.
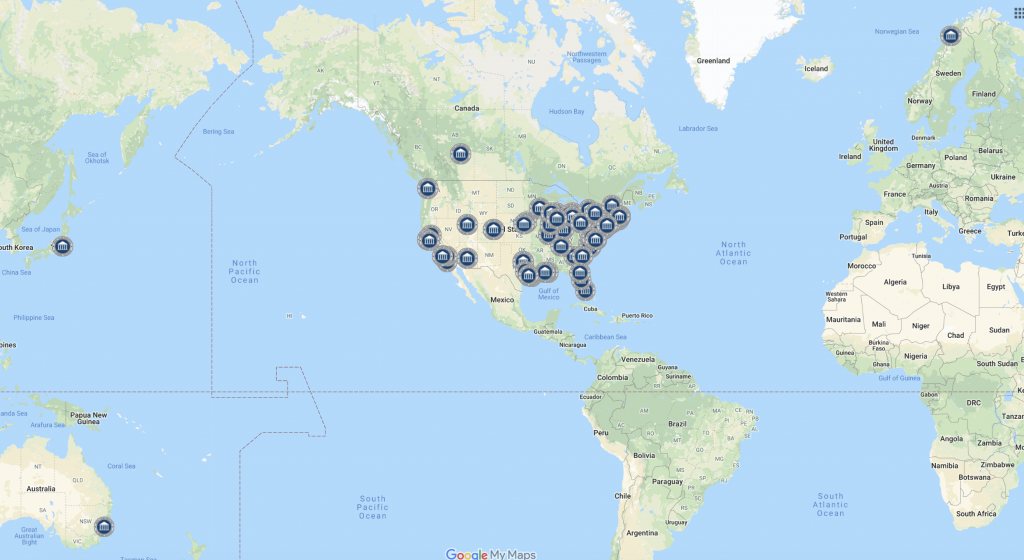
To efficiently and effectively advance this work on a national scale, the High Value Practice Academic Alliance was established in 2017, and 100 large and small teaching hospitals partner institutions representing >30 different medical specialties & subspecialties joined the organization. After 6 years of successful collaboration to gain expertise and compile educational resources, membership was opened to any medical center as the High Value Practice Alliance, with the mission of engaging practices, hospitals and systems in all settings in the learning network.

Architecture of High Value Health Care
A strategic plan is essential to ensure the quality, safety, and effectiveness of a new high value model for health care delivery. “Value” has been defined in various ways, with costs as the universal denominator and more recently cost-effectiveness as the numerator. Early and efficient diagnosis and management, patient safety, patient experience and disease prevention are key elements of the cost-effectiveness, underscoring the importance of quality-driven care refinement and systematic analyses to measure outcomes. To effectively refine medicine, performance improvement efforts must be implemented across 8 pillars:
-
-
- Diagnostic and therapeutic efficiency
- Care pathways to reduce unwarranted variation
- Care transitions including hospital discharge
- Optimizing patient care setting to reduce avoidable ED and hospital use
- Preventive medicine and healthy lifestyle
- Reduce inequities in high value care
- Foster interprofessional team building for optimal care delivery
- Educate trainees and practicing clinicians in principles of high value practice
-
While many different organizations are contributing to these efforts, the transition will only be successful if medical providers are accountable for improving the value of the care they deliver and join the charge to advance value-based quality-improvement. In the words of Richard Duszak, MD, former Director of Health Policy and Practice in the Emory Department of Radiology and current Professor and Chair of the Department of Radiology at the University of Mississippi Medical Center and Chair of the ACR’s Commission for Leadership and Practice Development , “Real innovation will only come from the ground up – from doctors and nurses and patients, and everyone else in the trenches.”






